In partnership with our parent organization, the International Center for Journalists (ICFJ), IJNet is connecting journalists with health experts and newsroom leaders through a webinar series on COVID-19. The series is part of the ICFJ Global Health Crisis Reporting Forum.
A year after COVID-19 was declared a national emergency, vaccines have finally arrived, with the U.S. averaging 2 million vaccine doses administered per day. But the arrival of vaccines also brings an explosion of information — some of it untrue. Dr. Galit Alter, a professor of medicine and a group leader at the Ragon Institute of MGH, MIT and Harvard, spoke with Patrick Butler, ICFJ’s Vice President of Content and Community, about vaccines.
How does the virus affect our system?
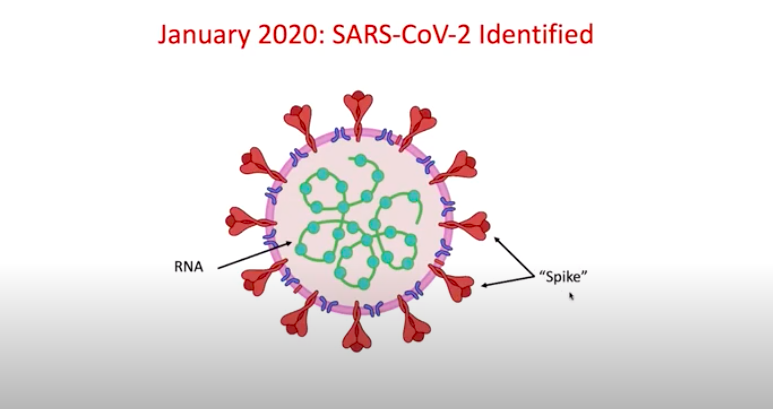
“While some vaccine developers decided to use the entire virus as a potential platform to drive immunity, most vaccine developers actually ended up focusing on a specific part of the virus, which is the Spike of the virus,” said Dr. Alter.
Dr. Alter explained that the virus causes COVID-19 disease through its ability to use the Spike protein to interact with a protein on the surface of our lung cells, called the ACE-2 receptor.
“Once that spike protein interacts with the ACE-2, this gives permission to the virus to now enter the cells where it can replicate, multiply and begin to spread and cause disease,” said Dr. Alter.This is the interaction that vaccine developers seek to block.
“What’s interesting about this particular ACE-2 receptor is that they are not only present on the surface of lung cells. They are also found in the gut, our blood vessel walls, heart cell wall and in some cells that live in our respiratory passageways, which allow us to smell and taste things,” she explains. This is why there are reports of people not being able to taste or smell when infected with the virus.
[Read more: Equity in vaccine access and distribution: Key takeaways]
How do vaccines work?
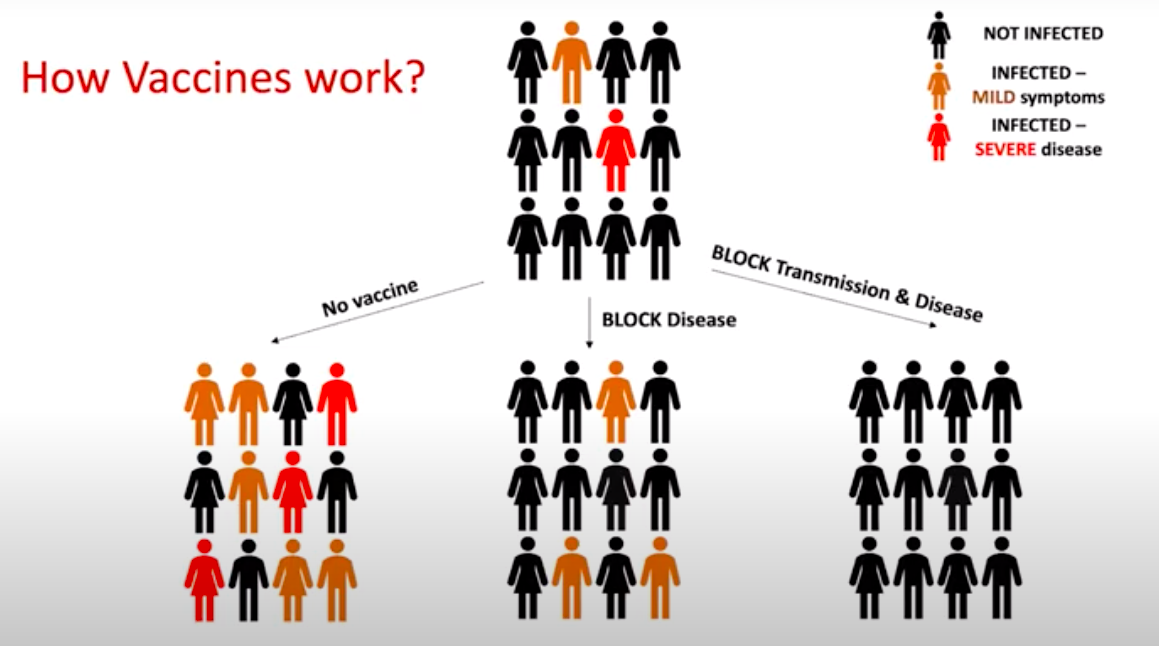
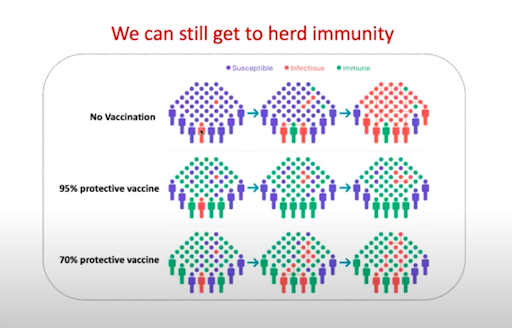
“Some vaccines will work by completely blocking infection,” explained Dr. Alter. This method is the most effective, as shown by the group on the right in the diagram above.
Another option, however, is using a vaccine to limit the severity of the disease in order to keep people out of hospitals and alive. “If we could turn COVID-19 into a cold for the whole world, I think we could live with that, right?” said Dr. Alter. “That would get us out of masks, back into our barbecues with our friends and back into churches, synagogues and mosques — wherever we wanted to go.”
[Read more: Tips to report on vaccine hesitancy]
What are the different types of vaccines?
The vaccine development community made a decision early on to focus on the Spike protein when developing vaccines, because this was the part of the virus that scientists believe “is the most important for antibodies to provide protection from infection,” said Dr. Alter.
Below is a breakdown of the different types of vaccines being used to fight COVID-19:
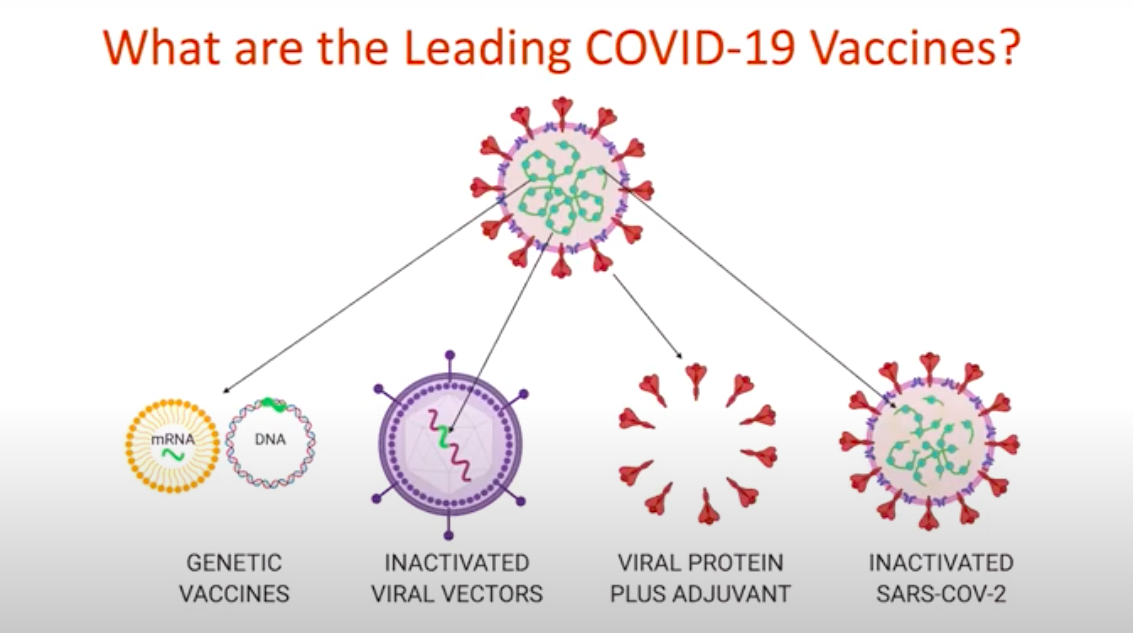
mRNA vaccines:
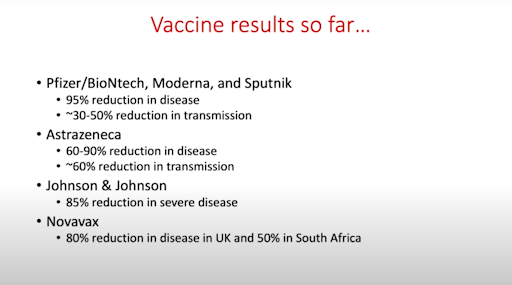
- The vaccines produced by Pfizer and Moderna are mRNA.
- “[mRNA vaccines] basically provide the software code for how to make these Spike proteins,” said Dr. Alter. “It leads the generation of proteins that are then released outside the cell. They get picked up by cells of the immune system that then tell those magical B cells — or antibody producing machines — to make lots of antibodies to fight the disease.”
- This is the first time mRNA vaccines are being used for large scale deployment to fight a single viral infection, but they’ve been developed for “dozens of years,” said Dr. Alter
Inactivated viral vector vaccines:
- These are the Adenoviral vaccines, such as the ones from Sputnik and Johnson & Johnson.
- They expose the body to the coronavirus Spike protein, which allows us to make antibodies to this target in a completely natural way.
- These vaccines can be produced at huge scales, which makes them advantageous over mRNAs to scale at a global level.
Inactivated SARS-COV-2:
- One current vaccine using this method is the Chinese Sinopharm vaccine.
- In this method the immune system is exposed to the entire virus in its intact form, but without the ability to cause infection.
- This type of vaccine is a little bit slower to produce because it requires the production of large amounts of the virus. Important chemical processes have to occur to make sure that the product is safe to go out.
Common questions:
Should people who have already had the disease, whether severe or mild, get vaccinated as well?
- “The bottom line is that even if you’ve had COVID-19 before, you have to get vaccinated and you should get both of the shots,” said Dr. Alter.
- She added: “There is data that’s emerging in the scientific community suggesting that, potentially, if you’ve had COVID-19, you might only need one shot. The problem is that natural immunity to COVID-19 is really heterogeneous — it’s so variable.”
- “If you have the option to get a COVID vaccine, get it,” she said. “And do the full regimen, don’t hesitate.”
How important is vaccinating children and when will we be able to do that?
- “There is zero question that if we don’t get into the pediatric population, we’re never going to get herd immunity,” said Dr. Alter. “That is a top priority from global communities and vaccine developers.”
- “There are pediatric trials that are starting across the globe. We are already working our way into the teenager population,” she said. “Soon enough, I think we’re going to get to the smaller kids and even potentially infants in the near future.”
Make sure to watch the webinar recording to learn more about how each vaccine works and more advice from Dr. Alter.
Lydia Antonio-Vila is a program assistant at ICFJ.
Main image CC-licensed by Unsplash via Renee Elias.

